What is the DASH diet?
The DASH Diet is a scientifically-backed eating pattern developed by the U.S. National Heart, Lung, and Blood Institute (NHLBI). The diet lowers high blood pressure and improves cardiovascular health.
Unlike restrictive fad diets, the DASH diet offers a flexible and sustainable lifestyle. Instead, it focuses on nutrient-rich whole foods while limiting foods that harm heart health. The American Heart Association (AHA) and NHLBI endorse it as first-line therapy for prehypertension and hypertension.
What does DASH stand for?
DASH stands for Dietary Approaches to Stop Hypertension.
The name reflects its primary purpose: managing high blood pressure through dietary changes.
Who should follow the DASH diet?
- People with high blood pressure
- The DASH diet helps control blood pressure. It is often the first treatment doctors recommend.
- People with slightly high blood pressure (pre-hypertension)
- The DASH diet helps stop blood pressure from getting worse.
- Anyone who wants a healthy heart
- Even if your blood pressure is normal, the DASH diet still supports heart health.
- People with a family history of heart disease
- The DASH diet lowers the risk of heart problems.
- People looking for a healthy diet they can follow long-term
- The DASH diet is flexible and easy to maintain over time.
- People with type 2 diabetes or at risk of diabetes
- The DASH diet helps control blood sugar and lowers the risk of diabetes.
Remember
DASH is safe for most people. However, people with serious kidney disease, electrolyte problems, or those taking certain medicines should talk to a doctor before starting it.
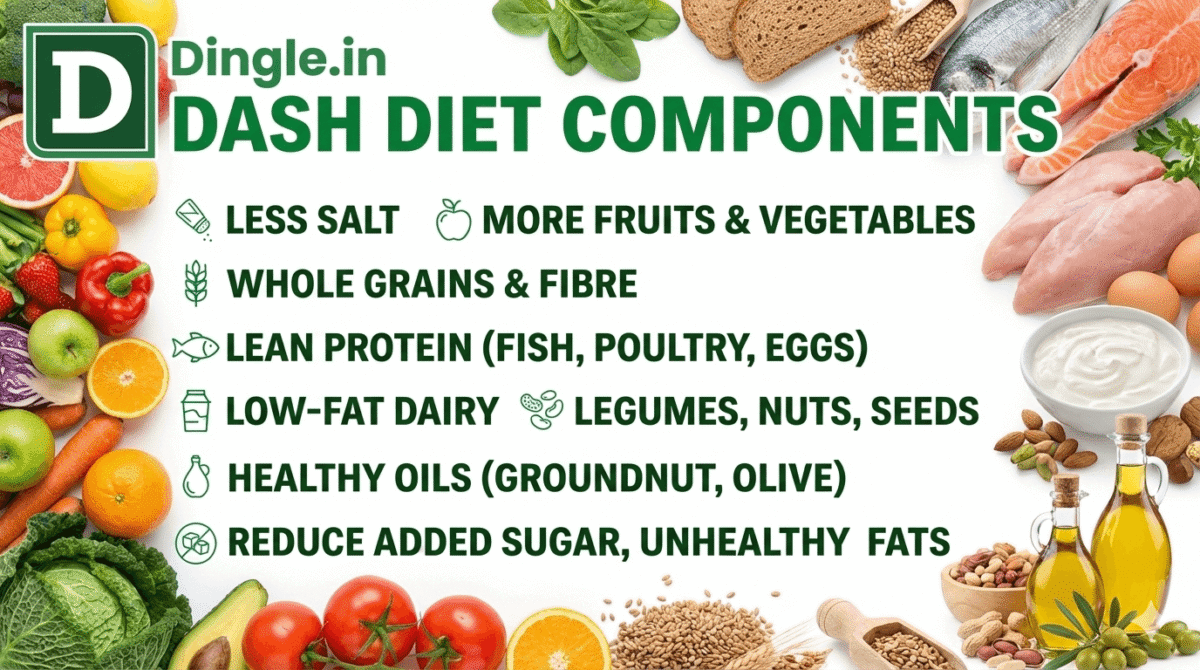
What are the components of DASH diet?
The DASH diet focuses on eating less salt and more healthy foods like fruits, vegetables, whole grains, low-fat dairy, and lean protein.at dairy, and lean protein.
- Cut down on unhealthy items. Reduce salt, added sugar, refined grains, and unhealthy fats.
- Prepare your meals around plant foods. Fill your plate with vegetables, fruits, and whole grains. This gives your body more fibre, vitamins, and minerals.
- Eat legumes, nuts, and seeds every day. Beans and lentils provide plant protein, while nuts and seeds supply healthy fats and fibre.
- Non-Vegetarian food eaters should choose lean protein sources. Eat fish (especially fatty fish), skinless chicken, and eggs. Eat red meat less often and choose lean, unprocessed fats when you do.
- Use healthy oils in small amounts. Cook with oils like groundnut oil. You may use olive, sunflower, or mustard oil; however, strictly avoid palm oil.
The DASH-Sodium Trial showed that combining DASH with sodium reduction produces even greater blood pressure lowering than either intervention alone.
Which foods are allowed on the DASH diet?
Vegetables:
Aim for a wide variety. Indian options include bhindi (okra), lauki (bottle gourd), palak (spinach), gajar (carrots), Baingan or Brinjal (eggplant or aubergine), and leafy greens.
Fruits:
Include diverse fresh fruits.
Examples: bananas, guava, papaya, apples, oranges, sweet limes. Eat Mangoes in moderation due to sugar content.
Whole Grains:
Choose atta roti (whole wheat flatbread) over maida, daliya (broken wheat), brown rice over white rice, oats, jowar (sorghum), bajra (pearl millet), ragi (finger millet).
Legumes, Nuts, Seeds:
Include diverse dals (moong, masoor, toor), rajma (kidney beans), chana (chickpeas), black-eyed peas, unsalted almonds, walnuts, flaxseed, chia seeds, and sunflower seeds.
Low-Fat Dairy:
Choose dahi/curd, skim milk, and low-fat paneer.
Lean Proteins:
Fish (rohu, surmai, pomfret), skinless poultry, eggs.
Healthy Oils:
Mustard oil, groundnut oil, sunflower oil, soybean oil, olive oil in modest quantities.
Which foods should you avoid on the DASH diet?
Sodium (Salt): Primary component to control blood pressure.
- WHO: Less than 2,000 mg sodium daily (approximately 5 grams salt, about 1 teaspoon)
- American Heart Association (AHA): Ideal of 1,500 mg daily, especially for those with or at high risk of hypertension
Added Sugars:
Minimise sweets, sugary beverages (sodas, sweetened juices), desserts, and hidden sugars in cereals, yoghurts, and sauces. Look for high-fructose corn syrup, sucrose, and dextrose on labels.
Saturated and Trans Fats:
Avoid fatty meat cuts, full-fat dairy (butter, ghee, full-fat paneer), tropical oils (coconut, palm), baked goods with shortening or hydrogenated oils.
Processed and Restaurant Foods:
Often high in hidden sodium, unhealthy fats, and added sugars. Prioritise home-cooked meals.
Is the DASH diet suitable for vegetarians or vegans?
Yes. Beans, seeds, and nuts are important parts of DASH, and meat substitutions work well using protein-rich non-animal products. DASH was designed to provide the blood pressure-reducing benefits of healthy vegetarian and vegan diets.
For vegetarians and vegans:
- Replace meat with legumes, tofu, tempeh
- Ensure adequate protein from varied plant sources
- Use calcium-fortified plant milks if avoiding dairy
- Consider B12 supplementation if fully vegan
The diet adapts easily to plant-based eating with its emphasis on vegetables, fruits, whole grains, legumes, nuts, and seeds.
How many servings of each food group should I eat on DASH diet?
Servings depend on daily calorie needs. For a 2,000-calorie diet:
- Grains: 6-8 servings (preferably whole grains)
- Vegetables: 4-5 servings
- Fruits: 4-5 servings
- Low-fat dairy: 2-3 servings
- Lean meats, poultry, fish: 6 ounces or less
- Nuts, seeds, legumes: 4-5 servings per week
- Fats and oils: 2-3 servings
- Sweets and added sugars: 5 servings or less per week
Serving examples:
- 1 slice bread or 1/2 cup cooked rice/pasta = 1 grain serving
- 1 cup raw leafy vegetables or 1/2 cup cooked vegetables = 1 vegetable serving
- 1 medium fruit or 1/2 cup fresh fruit = 1 fruit serving
- 1 cup milk or yogurt = 1 dairy serving
- 1 ounce cooked meat = 1 protein serving
The NHLBI provides free, detailed serving tables for different calorie levels (1,600 to 3,100 calories).
Important Considerations for Indian Food
Hidden Sodium Sources: Indian cuisine contains high sodium in:
- Pickles (achar)
- Papad (poppadums)
- Chutneys and ready-made masalas (especially chaat masala)
- Ketchup and store-bought sauces
- Packaged namkeen (savoury snacks)
- Instant noodles and ready-to-eat meals
- Restaurant gravies and curries
- Processed cheeses and some bread
Use these sparingly. The Government of India’s Eat Right India initiative offers tips for reducing salt.
Local Flavour Swaps: Enhance flavour without excessive salt:
- Acids: Lemon juice, lime juice, amchur (dried mango powder), kokum, vinegar
- Aromatics: Fresh garlic, ginger, green chillies
- Herbs: Fresh cilantro (dhania), mint (pudina), curry leaves
- Spices: Cumin (jeera), coriander (dhania), turmeric (haldi), asafoetida (hing), fenugreek (methi), black pepper
Prioritise Homemade Meals: Home cooking gives complete control over salt and oil content. Avoid packaged and ultra-processed foods with hidden sodium, unhealthy fats, and added sugars.
Smart Oil Choices: Choose mustard, groundnut oil. You can also take sunflower, or olive oil. Use sparingly. Avoid reusing cooking oil.
Dairy Choices: Use low-fat or fat-free dahi (curd) and milk. Choose low-fat paneer, enjoyed in moderation.
Example Daily Indian Menu (Approx. 2,000 kcal; ~1,500-2,000 mg sodium)
Breakfast: Vegetable Upma (whole wheat semolina, minimal salt, loaded with vegetables), 1 bowl low-fat dahi, fresh papaya or banana
Morning Snack: Roasted unsalted chana, 1 fresh orange
Lunch: 2 atta rotis (no added salt), mixed-vegetable sabzi (minimal oil and spices), moong dal (light tadka, minimal salt), cucumber-carrot-tomato salad with lemon-coriander dressing, 1 cup low-fat chaas (no added salt)
Evening Snack: Small handful of unsalted almonds, plain buttermilk or water
Dinner: Brown rice, rajma (pressure-cooked with spices, minimal salt), bhindi stir-fry (less oil), large mixed green salad
Optional Dessert: Fresh fruit bowl with seasonal fruits
Proven Benefits (Evidence-Supported)
Consistent Blood Pressure Reduction:
Reliably lowers blood pressure across diverse populations. More pronounced in people with hypertension.
Enhanced with Sodium Reduction:
Overall, combining the DASH diet with reduced salt intake lowers blood pressure more than either approach alone.
Improved Lipid Profiles:
Reduces LDL cholesterol and triglycerides in many people. Modified DASH reduces waist circumference and improves insulin sensitivity.
Cardiovascular Risk Reduction:
Strong evidence for blood pressure improvement. Promising long-term effects on preventing heart attack and stroke through improved blood pressure, lipids, and weight management.
Cancer Risk Reduction:
Associated with a lower risk of colorectal, breast, endometrial, and lung cancer.
Metabolic Syndrome Prevention:
Reduces metabolic syndrome risk by nearly 50%.
Key Benefits:
- Blood pressure reductions within weeks
- Additive benefit with sodium restriction
- Increased intake of fibre, potassium, magnesium, and calcium
- Reduced added sugars and unhealthy fats
- Lower risk of heart disease, stroke, and kidney disease
- Improved blood lipid profiles
- Sustainable, flexible eating pattern
How DASH Lowers Blood Pressure
DASH diet works through multiple mechanisms:
Increased Blood Pressure-Lowering Nutrients:
- Potassium: Counteracts sodium effects, promotes vasodilation, and helps the kidneys excrete excess sodium
- Magnesium: Relaxes blood vessel walls, regulates blood pressure through vasodilatory substances
- Calcium: Essential for blood vessel contraction and relaxation, maintains proper vascular tone
- Fibre: Lowers LDL cholesterol, improves blood sugar regulation, supports a healthy gut microbiome
Reduced Blood Pressure-Elevating Components:
- Sodium: High intake causes fluid retention, increasing blood volume and pressure
- Saturated Fat: Raises LDL cholesterol, leads to plaque buildup in arteries
- Added Sugars: Causes weight gain, insulin resistance, and chronic inflammation
Blood pressure reductions appear within 2 weeks of starting DASH. Benefits continue and often enhance over time, particularly in people with existing hypertension.
How much salt (sodium) can I have per day?
Standard DASH diet program allows up to 2,300 mg of sodium per day. Lower-sodium DASH restricts to 1,500 mg daily.
Overall, research shows that lowering salt intake leads to greater blood pressure reduction; however, the benefits for healthy people remain less clear.
India’s average daily salt intake is 8-11 grams per day, significantly exceeding WHO’s 5-gram recommendation. Conscious salt reduction is critical for the Indian population.
How quickly will I see results (lower blood pressure)?
Blood pressure reductions occur within two weeks of starting DASH diet.
Many people notice improvements within the first week.
Results vary based on:
- Baseline blood pressure (higher baseline = greater reduction)
- Adherence to the diet
- Sodium restriction level
- Individual factors (age, genetics, medications)
In particular, people with hypertension see more dramatic results compared to those with normal blood pressure. Combining DASH with sodium reduction produces faster, more substantial blood pressure lowering.
For maximum benefit, commit to DASH for at least 4-8 weeks while monitoring your blood pressure regularly.
Medical Trial findings and results.
A 1997 New England Journal of Medicine trial demonstrated DASH’s effectiveness compared to a typical U.S. diet.
Change on Blood pressure
- Overall: 5.5 mmHg drop in systolic pressure, 3.0 mmHg drop in diastolic
- Hypertensive individuals: 11.4 mmHg drop in systolic, 5.5 mmHg drop in diastolic
Can I drink coffee or alcohol on the DASH diet?
Coffee: DASH doesn’t specifically address caffeine consumption, as its influence on blood pressure remains unclear. Coffee can cause temporary blood pressure rises.
If you have high blood pressure or concerns about caffeine, discuss with your doctor.
You don’t need to eliminate caffeinated beverages. Up to 2 cups daily is generally acceptable, preferably unsweetened.
Alcohol: The Dietary Guidelines for Americans recommends that men limit alcohol to no more than two drinks daily and women to one or less. Drinking too much alcohol increases blood pressure.
For best results, limit alcohol consumption. If you drink, do so in moderation and not daily.
Can the DASH diet help with weight loss?
Yes, though DASH wasn’t designed specifically for weight loss. Many people lose weight on DASH because it eliminates high-fat and sugary foods, naturally reducing calorie intake.
Studies show people on DASH lose approximately 3.1 pounds over 8-24 weeks. Weight loss enhances blood pressure benefits, but DASH lowers blood pressure even without weight loss.
For weight loss on DASH:
- Choose lower calorie targets (1,600-1,800 calories)
- Increase physical activity
- Use smaller portions
- Focus on filling, low-calorie foods (vegetables, fruits, whole grains)
Do I need to exercise while following the DASH diet?
Exercise isn’t required for DASH to lower blood pressure, but combining diet with physical activity produces better results.
In addition, DASH recommends at least 30 minutes of exercise on most days of the week, which results in a total of about 2 hours and 30 minutes per week at moderate intensity.
For weight management, aim for 60 minutes daily. Activities include:
- Brisk walking
- Swimming
- Cycling
- Dancing
- Gardening
You can break exercise into three 10-minute sessions throughout the day. Start slowly and build up gradually. Choose activities you enjoy to maintain consistency.
Is the DASH diet suitable for people with diabetes or other conditions like Heart disease?
Diabetes:
Yes. DASH improves insulin sensitivity and glycemic control. Research suggests DASH decreases type 2 diabetes risk by 20%. The diet helps manage blood sugar through high fibre content and reduced refined carbohydrates.
Heart Disease:
Ideal for those with or at risk of heart disease. Importantly, DASH reduces cardiovascular risk factors such as high blood pressure, high cholesterol, and inflammation.
Kidney Disease:
Consult your doctor first. People with advanced chronic kidney disease may need to limit potassium, phosphorus, and protein. Standard DASH may not suit those on dialysis.
Gout:
DASH reduces gout risk. The diet’s emphasis on low-fat dairy and plant-based proteins benefits those with or at risk of gout.
Always consult your healthcare provider before starting DASH diet if you have existing health conditions or take medications.
Are there any side effects of DASH diet?
DASH has minimal side effects. The original trial reported side effects were negligible, with some subjects reporting constipation. Interestingly, the DASH diet reduced constipation compared to control diets.
Potential minor issues:
Digestive discomfort:
Rapid fibre increase causes bloating, gas, and discomfort. Solution: Increase fibre gradually, drink plenty of water.
Initial adjustment period:
However, some people experience hunger initially when reducing portion sizes or eliminating familiar foods. This typically resolves within 1-2 weeks.
Cost considerations:
Fresh produce and lean proteins cost more than processed foods. Solutions: Buy seasonal produce, use frozen or low-sodium canned options, and plan meals to reduce waste.
Potassium concerns:
Those with kidney problems must monitor potassium intake, as DASH is high in potassium-rich foods. Consult your doctor if you have kidney disease.
For most healthy people, DASH is safe and well-tolerated with no serious adverse effects.
Practical Steps for Adoption
1. Set Sodium Target:
Start with less than 2,300 mg of sodium daily. Gradually work toward 1,500 mg if feasible. Read food labels diligently.
2. Use the Plate Method:
Fill half your plate with vegetables and fruits, one-quarter with whole grains, and one-quarter with lean protein. Add low-fat dairy.
3. Plan Healthy Snacks:
Choose fruit, unsalted nuts, roasted chana, vegetable sticks with low-sodium dip, and low-fat dahi.
4. Season Smartly:
Use herbs, spices, citrus juices, garlic, ginger, and vinegars instead of salt. Experiment with salt-free spice blends.
5. Track Progress:
Monitor blood pressure regularly at home. Discuss progress and challenges with your doctor or dietitian.
6. Hydrate with Water:
Make water your primary beverage. Limit sugary drinks.
7. Transition Gradually:
Don’t change everything overnight. Add one extra vegetable serving daily, swap white bread for whole wheat, or reduce salt in one meal. Small, consistent changes accumulate.
Combining DASH with Other Lifestyle Practices
For optimal results, integrate DASH with:
- Sodium Reduction: Consistently reduce dietary sodium
- Regular Physical Activity: 150 minutes moderate-intensity aerobic exercise or 75 minutes vigorous-intensity exercise weekly
- Adequate Sleep: 7-9 hours of quality sleep nightly
- Stress Management: Meditation, yoga, deep breathing
- Limited Alcohol: Up to one drink daily for women, two for men (if consumed)
- Smoking Cessation: If applicable
- Medication Adherence: When prescribed by your healthcare provider
Conclusion
DASH diet is one of the most rigorously tested, scientifically validated diet plan for lowering blood pressure and improving diet quality. Benefits extend beyond blood pressure control to improved cholesterol, better metabolic health, and reduced chronic disease risk.
Start with manageable changes: incorporate more plant-based foods, fresh fruits, vegetables, and whole grains. Reduce salty, sugary, and fatty processed foods. Use free resources and comprehensive menus from NHLBI and other health organisations to make DASH practical, delicious, and sustainable.
DASH diet is an investment in your long-term health that delivers real, lasting benefits.
Take care.
References (Open-Access or Official)
- NHLBI (National Heart, Lung, and Blood Institute – National Institutes of Health): The primary source for comprehensive DASH Eating Plan overviews, detailed guides, serving tables, and sample menus. Their resources are often freely available online.
- NEJM Randomised Trials: The original DASH trial (1997) and the DASH-Sodium trial (2001) published in the New England Journal of Medicine provide the foundational, peer-reviewed evidence for the diet’s efficacy.
- AHA (American Heart Association): It Offers extensive recommendations on the DASH diet for blood pressure management, specific sodium targets, and overall heart-healthy eating guidelines.
- Cochrane (2025): Systematic reviews from Cochrane Library provide high-level evidence summaries on the DASH diet’s impact on cardiovascular health outcomes. (Note: “2025” implies a hypothetical future review or general reference to ongoing reviews.)
- ICMR-NIN (Indian Council of Medical Research – National Institute of Nutrition, India, 2024): It Offers specific Dietary Guidelines for Indians, including advice on salt reduction, healthy plate compositions, and adapting healthy eating patterns to the Indian cultural and culinary context. (Note: “2024” implies a hypothetical recent update or general reference to their current guidelines.)
- WHO (World Health Organisation, 2025): Publishes fact sheets and guidelines on sodium reduction, outlining global recommendations for adult sodium intake and strategies for population-level salt reduction. (Note: “2025” implies a hypothetical future publication or general reference to their current guidelines.)